Opinion: Pills for profit — unsafe medicines stay legal in India
Pharma companies often exploit the dual Centre-State approval system at the cost of risking people’s lives

By Nripendra Abhishek Nrip
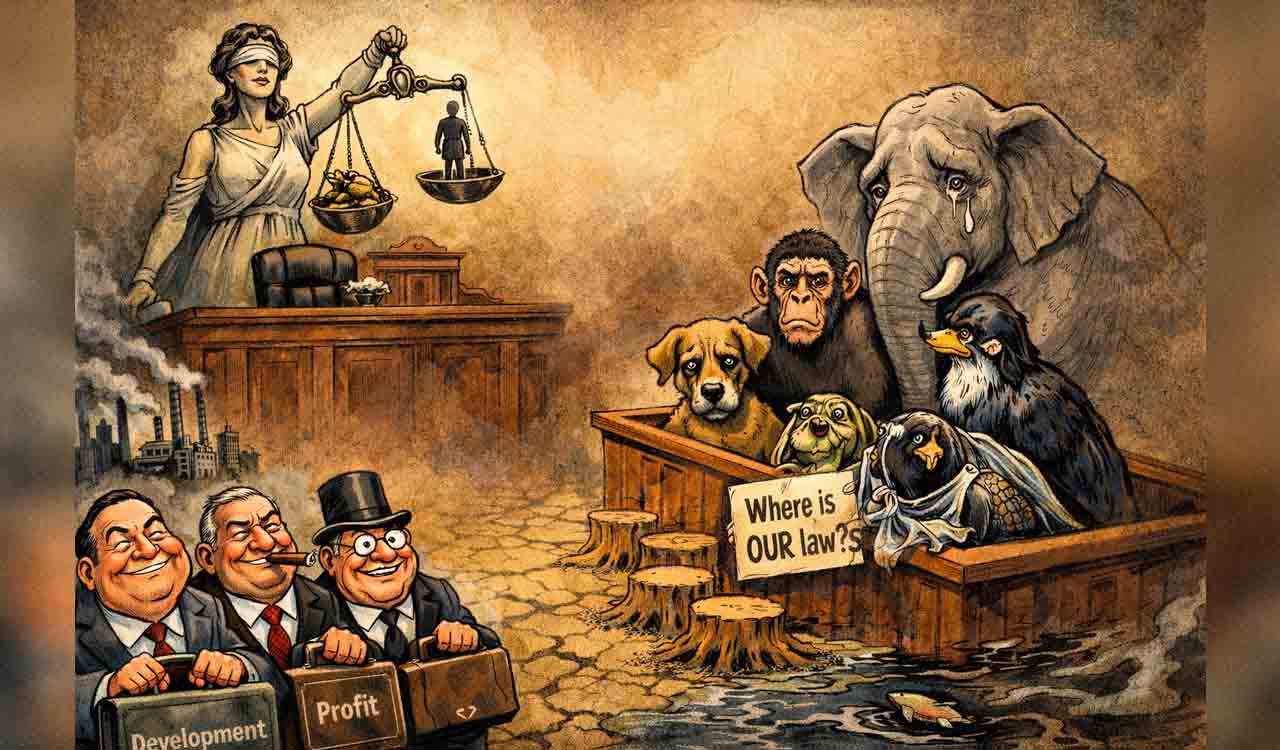
Medicines are one of the greatest gifts of science, saving countless lives and empowering humanity to fight severe diseases. Yet, when these very medicines become weapons in the blind race for profit, they cease to be science and instead turn into mere commerce, a trade where a handful of companies earn billions at the cost of risking people’s lives.
Also Read
Recently, a significant intervention occurred in India when the Central Drugs Standard Control Organisation (CDSCO) banned 35 ‘Fixed-Dose Combination’ (FDC) medicines. This decision is not only a bold move but also sets an important precedent for protecting public health.
Troubling Questions
Many of these banned medicines had been widely used for years to treat common ailments such as fever, pain, allergies, and colds. This raises pertinent questions: Was there no scientific evaluation before these drugs were allowed in the market? If there was an evaluation, why are these drugs now considered dangerous? And if there wasn’t any evaluation, how were these medicines available for so long?
These questions reveal the complex realities of drug regulation in India, the efficacy of regulatory agencies, the influence of pharmaceutical companies, and the inherent weaknesses in policymaking.
FDC drugs are formulations where two or more active pharmaceutical ingredients are combined in a single pill or syrup. Sometimes, FDCs offer therapeutic convenience, particularly for diseases like diabetes, tuberculosis, or HIV/AIDS, where multiple medications are needed simultaneously. However, often pharmaceutical companies exploit FDCs to boost profits. They combine various ingredients without scientific evidence or medical necessity and aggressively market them.
Many of these FDCs provide no added therapeutic advantage and, worse, sometimes increase the risk of side effects and complications. For example, drugs that mix a painkiller with an antibiotic or a steroid without medical justification are administered to patients, leading not only to deteriorating health but also contributing to the growing problem of Antimicrobial Resistance (AMR) — now a global health crisis.
Complex System
The history of FDC drug production and sale in India is riddled with complexities. The drug regulation system is divided between the Centre and the States. New drugs require approval from the central body (CDSCO), while manufacturing and distribution permissions are granted by the State drug controllers.
Pharmaceutical companies often exploit this confused setup by obtaining State approvals without securing central clearance, allowing them to sell their products for years without rigorous scientific vetting. This dual system creates a situation where drugs remain legally available in the market even if they are scientifically unsafe.
Dr Jyoti Singh asserts that banning these drugs, in reality, serves little tangible benefit. In her view, nowadays, even ‘bans’ have become a kind of business strategy, a clever ploy through which governments and pharmaceutical companies can earn even more profit.
India must overhaul its regulatory framework, with rigorous pre-approval evaluations and relentless post-market surveillance
Earlier, a single pill used to contain three or four active ingredients together, sufficient for treatment. Now, after banning such combinations, patients are required to take three separate pills containing the same ingredients individually, significantly increasing both the cost burden on patients and the profits for companies.
In 2016, the Ministry of Health appointed an expert committee, headed by Dr Chandrakant Kokate, to examine nearly 6,000 FDCs. The committee found that many of them had neither been approved on any sound medical basis nor subjected to adequate evaluation. It recommended an immediate ban on hundreds of FDCs.
Following this, some drugs were banned, but pharmaceutical companies fought lengthy legal battles to stall these bans. Eventually, the Supreme Court ruled that the decision regarding which drugs should be banned must be based on scientific evaluation by the CDSCO. The recent order is the outcome of that process. However, it also highlights a critical flaw: as long as there is a long gap between scientific evaluation and regulatory action, unsafe drugs will continue reaching the masses.
Thus, if a medicine is banned only after 15-20 years of use, a crucial question arises: who will compensate for the harm caused in that duration? Will pharmaceutical companies be held accountable? Will the government step forward through public interest litigations to ensure compensation for affected patients?
The Invisible Victim
There is an urgent need for a transparent system regarding the production, pricing, promotion, and distribution of medicines. Today, pharmaceutical companies heavily influence doctors through medical representatives to push their products. Patients trust their doctors and consume the prescribed medicines without knowing whether they were truly necessary. If doctors themselves are unaware of a drug’s effectiveness, the patient becomes a target of blind experimentation. This is why even ineffective or harmful drugs continue to be sold openly.
The commercialisation of healthcare services has worsened this crisis. In the mad race for profits, not just pharmaceutical companies but pharmacies, hospitals, and even doctors are increasingly drawn into a web of commercial interests. In a country like India, where a large population remains poor and illiterate, the sole aim of medical services should be public welfare, not profit-making.
However, when drug availability in public hospitals declines, forcing people into the expensive private sector, pharmaceutical companies find immense opportunities to maximise their profits — often at the cost of people’s health.
Another alarming aspect is the lack of public awareness. Even today, a significant number of people consume medicines without consulting doctors. They purchase Over-The-Counter (OTC) drugs, where sometimes even the shopkeepers recommend medicines without sufficient knowledge. To curb this trend, stricter laws are needed, but more importantly, large-scale public awareness campaigns must also be launched.
On the other hand, pharmaceutical companies argue that before banning any drug, a thorough scientific evaluation should be conducted. They also claim that sometimes, the regulatory bodies draw conclusions based on superficial testing, creating uncertainty and confusion in the pharmaceutical industry. This hampers innovation and research as well.
Call for Reform
There is a need for a regulatory process that is transparent, evidence-based, and fair. Any decision regarding banning a drug should not stem from political pressure or public emotion but should be grounded in scientific evidence.
It is also true that India is the largest producer of generic medicines in the world, and Indian-made drugs are considered affordable and accessible globally. However, if issues of quality and safety are ignored in this quest for supremacy, the very image of India as the ‘Pharmacy of the World’ could be jeopardised.
Therefore, India must strengthen its regulatory framework to ensure rigorous pre-approval evaluations but also maintain continuous post-market surveillance.
Banning dangerous drugs is not merely a matter of issuing government orders. It must be a collective effort encompassing health policy, ethical considerations, scientific scrutiny, and public interest. Until pharmaceutical companies are held accountable, the role of doctors becomes transparent, and the government assumes its responsibilities with seriousness, regulation will remain confined to paper.
(The author is a researcher based in Saran, Bihar)
Related News
-
Odisha government reviews protection of Lord Jagannath temple lands
8 hours ago -
Iran holds military drills with Russia as US carrier moves closer
8 hours ago -
This is taxpayers’ money: Supreme Court raps freebies culture
9 hours ago -
Hyderabad: Residents oppose Gandhi Sarovar Project over ‘forcible’ land acquisition
9 hours ago -
Australia level series as Indian women slide to 19-run defeat in second T20I
9 hours ago -
Karnataka beat Uttarakhand in semis, to face Jammu and Kashmir in Ranji final
9 hours ago -
Five Osmania varsity players in South Zone squad for Vizzy Trophy
9 hours ago -
Disciplined West Indies bundle out Italy with ease, tops Group C in T20 WC
9 hours ago